This 1-tissue compartment model has been developed by DeGrado et al. [30] for cardiac PET studies using 13NH3 ammonia bolus injection.
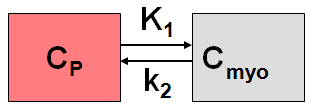
It includes a linear metabolite correction and describes the exchange of the NH3 between blood and the myocardium by the following differential equation
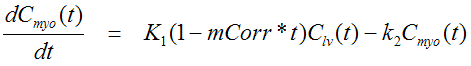
The factor mCorr represents the metabolite correction factor. A value of 0.077 [1/min] has been found for mCorr in humans [30].
Additionally, the model incorporates a cardiac dual spillover correction by the operational equation
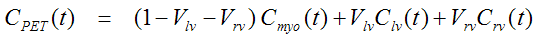
where
Vlv = spill-over fraction of the blood activity in the left ventricle Clv(t),
Vrv = spill-over fraction of the blood activity in the right ventricle Crv(t) .
DeGrado et al. recommend to only use the first 4 minutes of data after injection of the tracer to reduce the effects of metabolite buildup and washout.
Implementation Notes:
Abstract [30]
"BACKGROUND: Although several modeling strategies have been developed and validated for quantification of myocardial blood flow (MBF) from 13N- labeled ammonia positron emission tomographic data, a comparison of noise characteristics of the various techniques in serial studies is lacking. METHODS AND RESULTS: Dynamic 13N-labeled ammonia positron emission tomographic imaging was performed at baseline and after pharmacologic stress in (1) single studies of four dogs with concomitant measurement of microsphere blood flow and (2) initial and follow-up studies of eight normal volunteers. Data were obtained from short-axis images for the blood pool and myocardial regions corresponding to the three arterial vascular territories. Indexes of MBF were obtained by four distinct techniques: (1) University of California, Los Angeles, two-compartment model, (2) Michigan two-compartment model, and (3) a one- compartment model with variable blood volume term. Coronary flow reserve (CFR) was measured as the ratio of stress/rest MBF. The estimated standard deviation of the measurement error for the relative change between studies of rest and stress MBF and CFR was determined for each technique. Estimates of MBF from all techniques showed good correlation with microsphere blood flow (r = 0.95 to 0.96) in canine myocardium. In human studies, similar mean estimates of MBF were found with all techniques. Techniques 1 and 3 showed the smallest interstudy variability in MBF and CFR. The estimated standard deviations for these techniques were approximately 20%, 30%, and 27% for rest MBF, stress MBF, and CFR, respectively. CONCLUSION: Noninvasive quantification of MBF and CFR from dynamic 13N-labeled ammonia positron emission tomography is most reproducible with technique 1 or 3. The ability to account for differences in myocardial partial volume gives preference to technique 3. However, substantial interstudy variability in regional MBF remains, suggesting the importance of procedural factors or real temporal fluctuations in MBF."